Health Information
The following health topics are discussed below:-
- Latex Allergy
- Blood Pressure Basics
- Stroke Recognition
- Avian Influenza
- H5N1 Health Risks
- Lyme Disease & Black Legged Ticks
- Latex Allergy
-
Allergies occur when the body comes in contact with a foreign material. The body often does not react to the foreign material at the first contact. A reaction may not occur until many contacts are made. Not all reactions are allergies.
Reactions on the skin are caused by many different materials. One material that may cause a reaction is LATEX. Latex comes from the sap of a rubber tree. Proteins attached to the latex cause allergies.
Latex exposure has increased in the last 15 years because health workers use gloves more often. Latex is in the gloves and the powder inside the gloves. The powder allows latex particles to go into the environment.
Some products that often contain latex include...
- pacifiers
- feeding nipples
- adhesives
- erasers
- disposable diapers
- elastic fabric
- gloves
- balloons
- balls
- masks
- rubber toys
- rubber mats
- foam rubber
- carpet backing
- condoms
- diaphragms
- tape
- bandages
Who is at risk of Latex Allergy?
People who have a history of allergic reactions. They may suffer from asthma, hay fever or eczema.
Workers employed in latex manufacturing, health care and dentistry where gloves are used often.
People who have had a lot of surgery, especially more than 10 procedures.
Children with spina bifida who have had a lot of surgery and urinary catheters.
People who have allergies to avocados, bananas, kiwi, passion fruit, potatoes, tomatoes, pineapples, grapes, apricots, cherries, peaches and chestnuts. This is because these plants share similar proteins to the rubber tree.
You may be sensitive to latex if you have had a reaction during surgery, dental visit or a test with injections or tubes or if you have had a reaction after putting on rubber gloves.
Common Skin Reactions to latex include...
- stinging
- burning
- itching
- swelling
- redness
- scaling
- blistering
Latex particles are often airborne and contact can cause selling of your eyelids, lips and throat. Trouble breathing of tightness, wheezing, coughing or hives.
If you suspect that you have a latex allergy call your family doctor and ask for a latex sensitivity test.
Alternatives to latex are available. look for a LATEX FREE designation on products like bandages and gloves. Examination gloves are also available in vinyl or nitrile.
- The Basics of Blood Pressure
-
What is blood pressure?
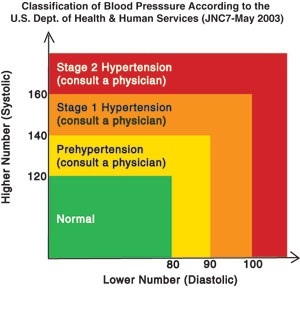
Simply put, blood pressure is a measurement of the force exerted on the arteries when the heart pumps blood through your body. Results are expressed in millimeters of mercury (mmHg), and written as a fraction with systolic over diastolic pressure. Normal blood pressure is about 120/80. Systolic blood pressure indicates the force applied when the heart pumps, while diastolic blood pressure is the force when the heart is at rest. Both of these values are important to your physician in order to assess your cardiovascular health.
What is hypertension?
Hypertension is the medical term for high blood pressure, and is a result of elevated systolic and/or diastolic levels. While hypertension is often linked to family history and lifestyle, it is not uncommon for doctors to be unable to pinpoint the cause. In fact, many people diagnosed with hypertension had no risk factors prior. Thus, the disease has come to be referred to as “the silent killer.” Left untreated, high blood pressure may lead to more serious problems, such as kidney disease, heart attack, or stroke. A home blood pressure monitor is an excellent way to track your blood pressure; however, only a qualified physician can safely and accurately interpret the readings obtained from your monitor. Never attempt self-diagnosis or treatment of your symptoms. High blood pressure is best controlled under the supervision of your doctor.
I took my blood pressure and it was high !!
Should I be scared?
Scared, no. Concerned, yes.
Many things can affect blood pressure, such as stress, excitement, exercise and medication. It can also vary widely from day to day, and even hour to hour. Blood pressure is considered to be high when the systolic reading is 140 mmHg or above or the diastolic number is 90 mmHg or higher for an extended period. Your doctor will be able to make the diagnosis after taking several readings over a period of time. Always consult with your doctor regarding concerns about your blood pressure.
Why take your blood pressure at home?
Several clinical studies have shown improvement in detection and treatment of hypertension among people using a home blood pressure monitor, in conjunction with advice from their doctor. Some patients are anxious while having their blood pressure taken in a doctor’s office or hospital. This can cause elevated readings referred to as “white coat hypertension.” Conversely, blood pressure measurement at home tends to be more relaxed, limiting “outside” influences. Thus, a truer blood pressure history may be obtained.
- STROKE RECOGNITION – 3 SIMPLE SIGNS
-
Ask a suspected Stroke victim to…
SMILE
RAISE BOTH HANDS
SPEAK A SIMPLE SENTENCE
Sometimes symptoms of a stroke are difficult to identify. Unfortunately, the lack of awareness can spell disaster. A stroke victim may suffer brain damage when people nearby fail to recognize the symptoms.
After discovering that a group of non-medical volunteers could identify facial weakness, arm weakness and speech problems, medical researchers urged the general public to learn these three questions. They presented their conclusions at the American Stroke Association's annual meeting (February 2004). They suggest that widespread use of this test could result in prompt diagnosis and treatment of the stroke and prevent brain damage.
Neurologists advise that the first three (3) hours after a stroke are critical to minimizing or preventing the potentially devastating effects of a stroke. The trick is recognizing that a stroke has occurred, and then getting medical attention to the patient within 3 hours, which is tough.
Doctors say a bystander can recognize a stroke by asking three simple questions:
1. *Ask the individual to SMILE.
2. *Ask the individual to RAISE BOTH ARMS.
3. *Ask the individual to SPEAK A SIMPLE SENTENCE (Coherently) (i.e. It is sunny out today)
If he or she has trouble with any of these tasks, call 9-1-1 immediately and describe the symptoms to the dispatcher.
- Avian Influenza (Bird Flu)
-
Key Facts About Avian Influenza (Bird Flu) and Avian Influenza A (H5N1) Virus
This fact sheet provides general information about avian influenza (bird flu) and information about one type of bird flu, called avian influenza A (H5N1), that has caused infections in birds in Asia and Europe and in humans in Asia. Also see Questions and Answers on the CDC website and Frequently Asked Questions (FAQs) on the World Health Organization (WHO) website.
Avian influenza in birds
Avian influenza is an infection caused by avian (bird) influenza (flu) viruses. These influenza viruses occur naturally among birds. Wild birds worldwide carry the viruses in their intestines, but usually do not get sick from them. However, avian influenza is very contagious among birds and can make some domesticated birds, including chickens, ducks, and turkeys, very sick and kill them.
Infected birds shed influenza virus in their saliva, nasal secretions, and feces. Susceptible birds become infected when they have contact with contaminated secretions or excretions or with surfaces that are contaminated with secretions or excretions from infected birds. Domesticated birds may become infected with avian influenza virus through direct contact with infected waterfowl or other infected poultry, or through contact with surfaces (such as dirt or cages) or materials (such as water or feed) that have been contaminated with the virus.
Infection with avian influenza viruses in domestic poultry causes two main forms of disease that are distinguished by low and high extremes of virulence. The “low pathogenic” form may go undetected and usually causes only mild symptoms (such as ruffled feathers and a drop in egg production). However, the highly pathogenic form spreads more rapidly through flocks of poultry. This form may cause disease that affects multiple internal organs and has a mortality rate that can reach 90-100% often within 48 hours.
Human infection with avian influenza viruses
There are many different subtypes of type A influenza viruses. These subtypes differ because of changes in certain proteins on the surface of the influenza A virus (hemagglutinin [HA] and neuraminidase [NA] proteins). There are 16 known HA subtypes and 9 known NA subtypes of influenza A viruses. Many different combinations of HA and NA proteins are possible. Each combination represents a different subtype. All known subtypes of influenza A viruses can be found in birds.
Usually, “avian influenza virus” refers to influenza A viruses found chiefly in birds, but infections with these viruses can occur in humans. The risk from avian influenza is generally low to most people, because the viruses do not usually infect humans. However, confirmed cases of human infection from several subtypes of avian influenza infection have been reported since 1997. Most cases of avian influenza infection in humans have resulted from contact with infected poultry (e.g., domesticated chicken, ducks, and turkeys) or surfaces contaminated with secretion/excretions from infected birds. The spread of avian influenza viruses from one ill person to another has been reported very rarely, and transmission has not been observed to continue beyond one person.
“Human influenza virus” usually refers to those subtypes that spread widely among humans. There are only three known A subtypes of influenza viruses (H1N1, H1N2, and H3N2) currently circulating among humans. It is likely that some genetic parts of current human influenza A viruses came from birds originally. Influenza A viruses are constantly changing, and they might adapt over time to infect and spread among humans.
During an outbreak of avian influenza among poultry, there is a possible risk to people who have contact with infected birds or surfaces that have been contaminated with secretions or excretions from infected birds.
Symptoms of avian influenza in humans have ranged from typical human influenza-like symptoms (e.g., fever, cough, sore throat, and muscle aches) to eye infections, pneumonia, severe respiratory diseases (such as acute respiratory distress), and other severe and life-threatening complications. The symptoms of avian influenza may depend on which virus caused the infection.
Studies done in laboratories suggest that some of the prescription medicines approved in the United States for human influenza viruses should work in treating avian influenza infection in humans. However, influenza viruses can become resistant to these drugs, so these medications may not always work. Additional studies are needed to demonstrate the effectiveness of these medicines.
Avian Influenza A (H5N1)
Influenza A (H5N1) virus – also called “H5N1 virus” – is an influenza A virus subtype that occurs mainly in birds, is highly contagious among birds, and can be deadly to them. H5N1 virus does not usually infect people, but infections with these viruses have occurred in humans. Most of these cases have resulted from people having direct or close contact with H5N1-infected poultry or H5N1-contaminated surfaces.
- Avian influenza A (H5N1) outbreaks
-
Human health risks during the H5N1 outbreak
Of the few avian influenza viruses that have crossed the species barrier to infect humans, H5N1 has caused the largest number of detected cases of severe disease and death in humans. In the current outbreaks in Asia and Europe more than half of those infected with the virus have died. Most cases have occurred in previously healthy children and young adults. However, it is possible that the only cases currently being reported are those in the most severely ill people, and that the full range of illness caused by the H5N1 virus has not yet been defined. For the most current information about avian influenza and cumulative case numbers, see the World Health Organization (WHO) avian influenza website.
So far, the spread of H5N1 virus from person to person has been limited and has not continued beyond one person. Nonetheless, because all influenza viruses have the ability to change, scientists are concerned that H5N1 virus one day could be able to infect humans and spread easily from one person to another. Because these viruses do not commonly infect humans, there is little or no immune protection against them in the human population. If H5N1 virus were to gain the capacity to spread easily from person to person, an influenza pandemic (worldwide outbreak of disease) could begin.
No one can predict when a pandemic might occur. However, experts from around the world are watching the H5N1 situation in Asia and Europe very closely and are preparing for the possibility that the virus may begin to spread more easily and widely from person to person.
Treatment and vaccination for H5N1 virus in humans
The H5N1 virus that has caused human illness and death in Asia is resistant to amantadine and rimantadine, two antiviral medications commonly used for influenza. Two other antiviral medications, oseltamavir and zanamavir, would probably work to treat influenza caused by H5N1 virus, but additional studies still need to be done to demonstrate their effectiveness.
There currently is no commercially available vaccine to protect humans against H5N1 virus that is being seen in Asia and Europe. However, vaccine development efforts are taking place. Research studies to test a vaccine to protect humans against H5N1 virus began in April 2005, and a series of clinical trials is under way.
Avian Influenza Infection in Humans
Although avian influenza A viruses usually do not infect humans, more than 100 confirmed cases of human infection with avian influenza viruses have been reported since 1997. For example, the World Health Organization (WHO) maintains situation updates and cumulative reports of human cases of avian influenza A (H5N1). Most cases of avian influenza infection in humans are thought to have resulted from direct contact with infected poultry or contaminated surfaces. However, there is still a lot to learn about how different subtypes and strains of avian influenza virus might affect humans. For example, it is not known how the distinction between low pathogenic and highly pathogenic strains might impact the health risk to humans. (For more information, see “Low Pathogenic versus Highly Pathogenic Avian Influenza Viruses” on the CDC Influenza Viruses Web page.
Because of concerns about the potential for more widespread infection in the human population, public health authorities closely monitor outbreaks of human illness associated with avian influenza. To date, human infections with avian influenza A viruses detected since 1997 have not resulted in sustained human-to-human transmission. However, because influenza A viruses have the potential to change and gain the ability to spread easily between people, monitoring for human infection and person-to-person transmission is important. (See Information about Influenza Pandemics for more information.)
Instances of Avian Influenza Infections in Humans
Confirmed instances of avian influenza viruses infecting humans since 1997 include:
* H5N1, Hong Kong, Special Administrative Region, 1997: Highly pathogenic avian influenza A (H5N1) infections occurred in both poultry and humans. This was the first time an avian influenza A virus transmission directly from birds to humans had been found. During this outbreak, 18 people were hospitalized and six of them died. To control the outbreak, authorities killed about 1.5 million chickens to remove the source of the virus. Scientists determined that the virus spread primarily from birds to humans, though rare person-to-person infection was noted.
* H9N2, China and Hong Kong, Special Administrative Region, 1999: Low pathogenic avian influenza A (H9N2) virus infection was confirmed in two children and resulted in uncomplicated influenza-like illness. Both patients recovered, and no additional cases were confirmed. The source is unknown, but the evidence suggested that poultry was the source of infection and the main mode of transmission was from bird to human. However, the possibility of person-to-person transmission could not be ruled out. Several additional human H9N2 infections were reported from China in 1998-99.
* H7N2, Virginia, 2002: Following an outbreak of H7N2 among poultry in the Shenandoah Valley poultry production area, one person was found to have serologic evidence of infection with H7N2.
* H5N1, China and Hong Kong, Special Administrative Region, 2003: Two cases of highly pathogenic avian influenza A (H5N1) infection occurred among members of a Hong Kong family that had traveled to China. One person recovered, the other died. How or where these two family members were infected was not determined. Another family member died of a respiratory illness in China, but no testing was done.
* H7N7, Netherlands, 2003: The Netherlands reported outbreaks of influenza A (H7N7) in poultry on several farms. Later, infections were reported among pigs and humans. In total, 89 people were confirmed to have H7N7 influenza virus infection associated with this poultry outbreak. These cases occurred mostly among poultry workers. H7N7-associated illness included 78 cases of conjunctivitis (eye infections) only; 5 cases of conjunctivitis and influenza-like illnesses with cough, fever, and muscle aches; 2 cases of influenza-like illness only; and 4 cases that were classified as “other.” There was one death among the 89 total cases. It occurred in a veterinarian who visited one of the affected farms and developed acute respiratory distress syndrome and complications related to H7N7 infection. The majority of these cases occurred as a result of direct contact with infected poultry; however, Dutch authorities reported three possible instances of transmission from poultry workers to family members. Since then, no other instances of H7N7 infection among humans have been reported.
* H9N2, Hong Kong, Special Administrative Region, 2003: Low pathogenic avian influenza A (H9N2) infection was confirmed in a child in Hong Kong. The child was hospitalized and recovered.
* H7N2, New York, 2003: In November 2003, a patient with serious underlying medical conditions was admitted to a hospital in New York with respiratory symptoms. One of the initial laboratory tests identified an influenza A virus that was thought to be H1N1. The patient recovered and went home after a few weeks. Subsequent confirmatory tests conducted in March 2004 showed that the patient had been infected with avian influenza A (H7N2) virus.
* H7N3 in Canada, 2004: In February 2004, human infections of highly pathogenic avian influenza A (H7N3) among poultry workers were associated with an H7N3 outbreak among poultry. The H7N3-associated, mild illnesses consisted of eye infections.
* H5N1, Thailand and Vietnam, 2004, and other outbreaks in Asia during 2004 and 2005: In January 2004, outbreaks of highly pathogenic influenza A (H5N1) in Asia were first reported by the World Health Organization. Visit the Avian Influenza section of the World Health Organization Web site for more information and updates.
Symptoms of Avian Influenza in Humans
The reported symptoms of avian influenza in humans have ranged from typical influenza-like symptoms (e.g., fever, cough, sore throat, and muscle aches) to eye infections (conjunctivitis), pneumonia, acute respiratory distress, viral pneumonia, and other severe and life-threatening complications.
Antiviral Agents for Influenza
Four different influenza antiviral drugs (amantadine, rimantadine, oseltamivir, and zanamivir) are approved by the U.S. Food and Drug Administration (FDA) for the treatment of influenza; three are approved for prophylaxis. All four have activity against influenza A viruses. However, sometimes influenza strains can become resistant to these drugs, and therefore the drugs may not always be effective. For example, analyses of some of the 2004 H5N1 viruses isolated from poultry and humans in Asia have shown that the viruses are resistant to two of the medications (amantadine and rimantadine). Also, please note the January 14, 2006 CDC Health Alert Notice (HAN), in which CDC recommends that neither amantadine nor rimantadine be used for the treatment or prevention (prophylaxis) of influenza A in the United States for the remainder of the 2005-06 influenza season. Monitoring of avian influenza A viruses for resistance to influenza antiviral medications is ongoing.
- Lyme Disease
-
Cases of Lyme disease surge in Ontario (November 2015)
Confirmed cases of Lyme disease in Ontario more than doubled this year as blacklegged ticks officially make Greater Toronto home. The National Microbiology Lab confirmed this week that for the second season in a row, a blacklegged tick infected with Borrelia burgdorferi — the bacterium that can cause potentially disabling disease in humans and pets alike — was found in Rouge Valley, which spans Durham, York and Toronto. “Once the ticks are established in the location... they don’t ever leave,” said Curtis Russell, an expert in vector-borne diseases at Public Health Ontario. “Now we just have to make sure to see where they’re expanding to.” Public health data show 304 confirmed cases and 54 probable cases of Lyme disease reported in Ontario between January and November this year. In 2014, 149 cases were confirmed and 71 were probable. Typical symptoms of infection can include fever, headache, muscle and joint pains, fatigue and skin rash. Untreated, the disease can last for years and cause neurological and musculoskeletal damage. In some cases, it can lead to heart infection and death. “Over the last few years, Lyme disease in Canada has evolved from an unusual and focal issue, to an emergent and expanding problem,” Health Canada warned in a recent report. What’s especially concerning is the spread of ticks from relatively isolated forests to more densely populated areas.
Prior to the mid-1990s, Lyme-diseased ticks were found in only one area in all of Canada — Long Point Provincial Park on Lake Erie. This year, 16 new risk zones were identified in Ontario alone, including Rouge Valley. The latest Toronto-specific data on human illness has not yet been compiled, but last year, Toronto Public Health reported 34 confirmed and four probable cases — the highest number in Ontario. That doesn’t mean, however, that all these people were exposed to the bacterium in Toronto. Ticks often travel on the bodies of migratory birds or white-tailed deer. Since the mid-1990s, parks
along the northern shores of Lakes Erie and Ontario have gradually become hotbeds for blacklegged ticks.
When travelling birds stop at these parks, the ticks fall off and look for new hosts. Ticks move very slowly. When they want to feed, they will climb to the tip of a grass blade and wait for an animal to latch onto. A tick can feed on the blood of a single host for days, even a week. If that tick is infected with Lyme, it will take 24 hours to transmit the bacteria from its gut to its salivary glands and into its host, which is why public health agencies urge people who visit leafy, tall-grassy areas to frequently check themselves and their pets for ticks.
At least 900 dogs across Ontario tested positive for Lyme disease this year — a sharp increase from just 91 cases in 2012, according to Idexx, which publishes data on pet disease. The cases are based on an annual, routine test administered to dogs at veterinary clinics. There are several labs that offer this testing, but only Idexx shares its results publicly.
Public Health Ontario reviews animal data, Russell said, but it’s just one piece of the puzzle. While the numbers seem high, dogs respond much differently to Lyme disease than humans. Dr. Andrew Peregrine, a clinical parasitologist at University of Guelph, estimates that only five per cent of infected dogs will develop clinical signs, which can include intermittent limping, swollen joints and lethargy, or more serious kidney problems. And while humans will typically show signs of infection within a week or two, two to five months may pass before a dog shows symptoms. Dr. Scott Stevenson sees between five and a dozen dogs each year that show clinical signs of Lyme
disease at his Thousand Islands veterinary clinic. In those cases, he recommends a full month of antibiotic treatment.
Mostly, though, he prescribes prevention strategies for pets and humans such as daily tick checks whenever the temperature is above freezing.
“There isn’t risk 365 days in Ontario, but there is risk in all 12 months of the year because there are days in January where it’s above 4 degrees Celsius and the ticks are out.”
There are no control measures for blacklegged ticks.
“The impact on the environment would be awful if you tried to get rid of them,” Peregrine says.
“We really need to start learning to live with them.”
At Queen’s Park on Thursday, NDP MPP Michael Mantha (Algoma-Manitoulin) criticized the health minister for failing to follow through on his commitment last year to create an action plan on Lyme disease.
“If the stakeholders are not consulted, we will get absolutely no changes made to Lyme education, testing and treatment, and patients will continue to suffer,” he said.
Humans and dogs heading into wooded areas across Ontario should know that blacklegged ticks can transmit Lyme disease at only two stages in their two-year life cycle.
The Tick Life Cycle
Eggs: An adult female tick that has fed on blood can produce thousands of eggs after mating inthe spring. A female infected with Lyme disease cannot pass the bacterium to her eggs.
Larva: Pinhead-sized larvae typically carry no risk of disease until they feed on a small mammal, often a mouse or bird, which can be infected with the bacterium Borellia burgdorferi that causes Lyme disease.
Nymph: By this stage, the tick may already carry the bacterium if it fed on an infected mammal in the larva stage. The size of a poppy seed, nymphs are prevalent in spring. They’re opportunistic and will feed on whatever walks by — small mammals, birds, dogs and people. The blood meal can last three to seven days, after which the fully engorged tick will drop to the ground and moult into its final life stage.
Adults: At their largest size in the life cycle, they’re roughly 3 mm unfed. Engorged, they can balloon to 10 mm, making them easier to see and pick off before they can transmit the bacterium to a person or dog. If an adult tick cannot find a host to feed on before winter, they will become relatively inactive under the snow and resume their search for a host when the temperature rises above zero.